A20 is a damaging regulator of NF-κB, and mutational loss of A20 expression is concerned in the pathogenesis of autoimmune illnesses and B-cell lymphomas. To make clear the function of A20 in grownup hematopoiesis, we generated conditional A20 knockout mice (A20(flox/flox) ) and crossed them with Mx-1Cre (MxCre (+)) and ERT2Cre (ERT2Cre (+)) transgenic mice in which Cre is inducibly activated by endogenous interferon and exogenous tamoxifen, respectively.
A20(flox/flox) MxCre (+) (A20Mx) mice spontaneously exhibited myeloid proliferation, B cell apoptosis, and anemia with overproduction of pro-inflammatory cytokines. Bone marrow transplantation demonstrated that these adjustments have been brought on by hematopoietic cells.
NF-κB was constitutively activated in A20Mx hematopoietic stem cells (HSCs), which precipitated enhanced cell cycle entry and impaired repopulating capacity.
Tamoxifen stimulation of A20(flox/flox) ERT2Cre (+) (A20ERT2) mice induced fulminant apoptosis and subsequent myeloproliferation, lymphocytopenia, and progressive anemia with extreme manufacturing of pro-inflammatory cytokines, as noticed in A20Mx mice.
These results exhibit that A20 performs important roles in the homeostasis of grownup hematopoiesis by stopping apoptosis and irritation. Our findings present insights into the mechanism underlying A20 dysfunction and human illnesses in which A20 expression is impaired.
Self-renewal is a defining attribute of stem cells; nonetheless, the molecular pathways underlying its regulation are poorly understood.
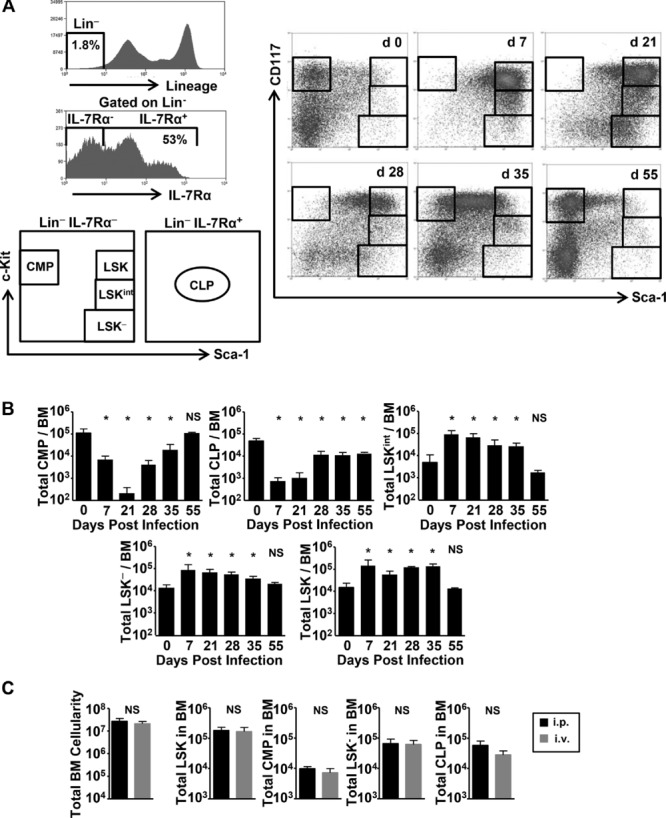
Here, we exhibit that conditional inactivation of the Pbx1 proto-oncogene in the hematopoietic compartment results in a progressive loss of long-term hematopoietic stem cells (LT-HSCs) that’s related to concomitant discount in their quiescence, resulting in a defect in the upkeep of self-renewal as assessed by serial transplantation.
Transcriptional profiling revealed that a number of stem cell upkeep elements are perturbed in Pbx1-deficient LT-HSCs, which prematurely specific a big subset of genes, together with cell-cycle regulators, usually expressed in non-self-renewing multipotent progenitors.
A big proportion of Pbx1-dependent genes is related to the TGF-beta pathway, which serves a significant function in sustaining HSC quiescence. Prospectively remoted, Pbx1-deficient LT-HSCs show altered transcriptional responses to TGF-beta stimulation in vitro, suggesting a doable mechanism by way of which Pbx1 upkeep of stem cell quiescence might in half be achieved.
Hoxb5 marks long-term haematopoietic stem cells and reveals a homogenous perivascular area of interest
Haematopoietic stem cells (HSCs) are arguably probably the most extensively characterised tissue stem cells. Since the identification of HSCs by potential isolation, advanced multi-parameter circulation cytometric isolation of phenotypic subsets has facilitated research on many elements of HSC biology, together with self-renewal, differentiation, ageing, area of interest, and variety.
Replacement of disease-causing stem cells
we exhibit by unbiased multi-step screening, identification of a single gene, homeobox B5 (Hoxb5, often known as Hox-2.1), with expression in the bone marrow that’s restricted to long-term (LT)-HSCs in mice. Using a mouse single-colour tri-mCherry reporter pushed by endogenous Hoxb5 regulation, we present that solely the Hoxb5(+) HSCs exhibit long-term reconstitution capability after transplantation in main transplant recipients and, notably, in secondary recipients.
Only 7-35% of numerous beforehand outlined immunophenotypic HSCs are LT-HSCs. Finally, by in situ imaging of mouse bone marrow, we present that>>94% of LT-HSCs (Hoxb5(+)) are immediately hooked up to VE-cadherin(+) cells, implicating the perivascular house as a near-homogenous location of LT-HSCs.
Replacement of disease-causing stem cells with wholesome ones has been achieved clinically through hematopoietic cell transplantation (HCT) for the final 40 years, as a therapy modality for a range of cancers and immunodeficiencies with reasonable, however growing, success.
This process has historically included transplantation of blended hematopoietic populations that embody hematopoietic stem cells (HSC) and different cells, equivalent to T cells. This article explores and delineates the potential enlargement of this system to deal with a range of inherited illnesses of immune function, the present boundaries in HCT and pure HSC transplantation, and the up-and-coming methods to fight these obstacles.
